Continuing the theme of notes on how to approach CT and MRI interpretation, here is the section on MR spine. MR spine took me quiet a bit of effort and a lot of time to get comfortable with. Hopefully, this will give you a better start.
ABCDE of MR Spine:
A: Alignment:
- Assess:
- Kyphosis, lordosis.
- For retrolisthesis, spondylolisthesis, spondylolysis.
- For ligamentous injury.
- Sequences to assess:
- Sag T1, Sag T2, Sag STIR,
- Axial T2, axial STIR
- Sag T1:
- Assess for retrolisthesis, spondylolisthesis, spondylolysis.
- Assess ligaments: ligamentum flavum and supraspinous ligament (continuous hyointense line).
- Sag T2, Sag STIR:
- Hyperintensity in ligamentous injury.
- Assess ligaments: ligamentum flavum and supraspinous ligament (continuous hyointense line).
- Interspinous ligament change (hyperintensity on sagittal T2, sagittal STIR).
- Assess: Anterior longitudinal ligament (ALL), Posterior longitudinal ligament (PLL), Ligamentum flavum, Articular facet capsules, Interspinous ligaments, Supraspinous ligament (connects the tips of the spinous processes from C7 to the sacrum), ligamentum nuchae.
- Axial T2, axial STIR:
- Facet edema or fluid (hyperintensity).
B: Bone:
- Sequences: Sag T1, Sag STIR, Sag T2, axial T2
- Bones to assess:
- Vertebral body, vertebral body endplates, pedicles, Pars Interarticularis (the part between the facet superior and inferior articular processes), laminae, transverse processes, spinous processes.
- Also skull, clivus, occipital condyle, Atlantooccipital joint (Occipital condyle- Lateral mass of C1), Odontoid process, arch of C1 (anterior and posterior),
- Bone edema suggests fractures or bone contusions.
- Assess vertebral endplates for degenerative changes (e.g. Modic changes)
- Marrow edema(T1 dark, T2 bright)
- Hematopoietic (Red) marrow to fatty (yellow) marrow conversion (T1 bright, T2 iso-bright)
- Subchondral bony sclerosis (T1 dark, T2 dark)
- Schmorl’s nodes
- Also assess ligamentous injury, assess: Anterior longitudinal ligament (ALL), Posterior longitudinal ligament (PLL), Ligamentum flavum, Articular facet capsules, Interspinous ligaments, Supraspinous ligament (connects the tips of the spinous processes from C7 to the sacrum).
C: Cord:
- STIR, T1
- Assess for spinal cord lesions, edema, expansion, cystic changes, syringomyelia, or atrophy, assess 3 columns for spinal instability (see Denis classification below)
D: Discs:
- Sequences to assess: AX T2, AX GRE, AX PD,
- Disc bulge vs. protrusion:
- Bulge (>180 degrees) vs. Herniated disc (<180 degrees). Types of Herniated discs: Protrusion (<90 degrees) vs. broad-based protrusion (90-180 degrees) vs. extrusion (longer than it is wide)
- In axial plane: central, right/left central, right/left sub-articular, right/left foraminal, right/left extra-foraminal
- In axial plane, canal stenosis:
- <1/3 mild, 1-2/3 moderate, >2/3 severe. Same grading for neuroforaminal stenosis
- Assess these structures:
- Ligamentum flavum, facet joints, neural foramena, central canal
E: Enhancement:
- T1+GAD
Editor note:
Approach to structures; sagittal, parasagittal and axial:
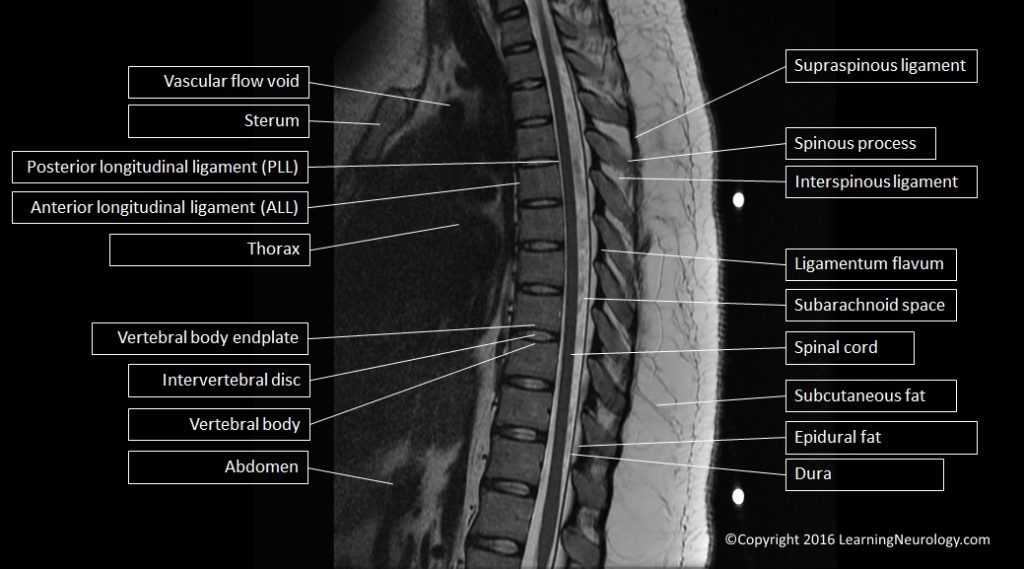
Approach to structures, sagittal:
Scroll and look at midline image (in the mid-sagittal plane) from bottom to top. Then look laterally at the parasagittal planes. Observe the normal and abnormal structures.


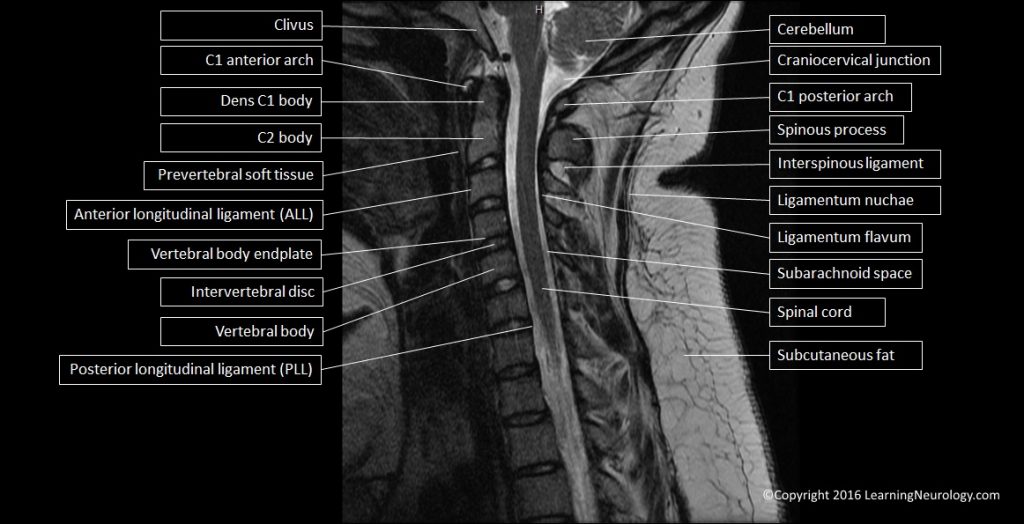

- Review the posterior fossa (medulla, pons, 4th ventricle, cerebellum)
- Craniocervical junction
- Anterior and posterior arch of C1
- C1 (dens-Odontoid) body
- C2 body
- Vertebral bodies
- Intervertebral discs
- Sacrum
- 3 Columns for spinal stability (anterior, middle and posterior)
- Anterior longitudinal ligament (ALL)
- Posterior longitudinal ligament (PLL)
- Spinal cord
- CSF space, spinal canal, subarachnoid space
- Posterior elements: spinous processes (C2-C7, thoracic, lumbar), interspinous ligaments, supraspinous ligament (C7 to sacrum, connects the tips of the spinous processes),
- Posterior soft tissues (cervical, thoracic and lumbar)
- Epidural fat
- Paraspinal muscle
- Prevertebral soft tissue
- Pharynx, epiglottis,
- Retropharyngeal space, pre-vertebral space
- Craniocervical junction ligaments:
- Anterior occipitoatlantal membrane (occipital bone to C1 arch anteriorly)
- Anterior atlantoaxial membrane (C1 arch anteriorly to C2 body)
- Apical ligament (Odontoid to clivus)
- Tectorial membrane (clivus to Odontoid, prolongation of posterior
- longitudinal ligament)
- Posterior atlantoaxial membrane (occiput to C1 arch posteriorly)
Parasagittal structures:
- Atlantooccipital joint (Occipital condyle- Lateral mass of C1)
- Atlanto-axial joint
- Facet joints and articular processes:
- Articular facet capsules
- Inferior articular process of C2
- Superior and inferiorarticular processes C3-C7, thoracic and lumbar
- Neuroforamen (Intervertebral foramen)
- Vertebral artery
- Lamina C3-C7, thoracic, and lumbar
Approach to structures, axial:
When interpreting the axial images follow a systematic approach. It is also useful to have two screens linked with the mid-line sagittal view to help you locate which axial slice level (vertebra or intervertebral disc) you are looking at. Scroll through the MRI from top to bottom while interpreting each of these systems or areas at a time. The vertebral column and ligaments, the CSF system, the spinal cord cord (grey matter structure and white matter structure), and adjacent tissues including pharynx and kidneys.




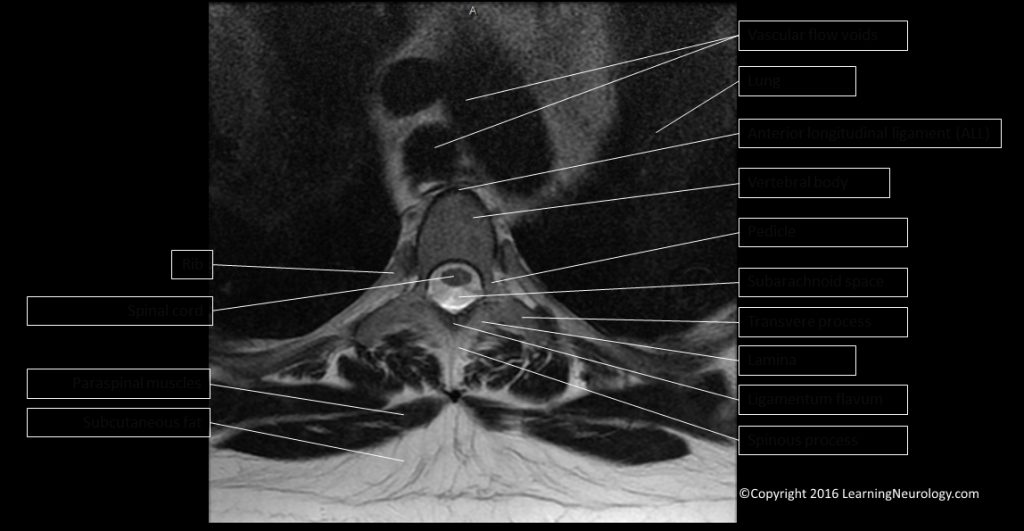
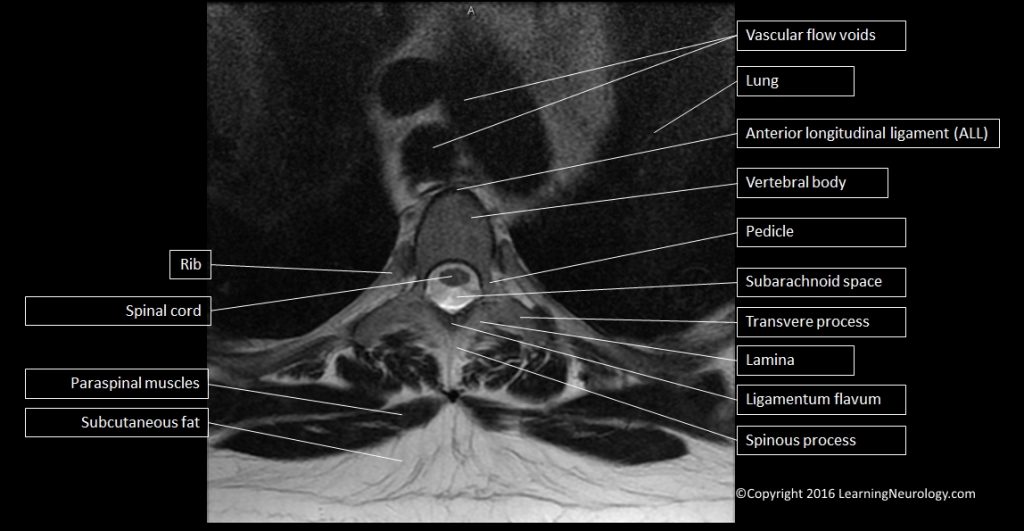
- CSF space
- Spinal cord
- Nerve root
- Intervertebral disc
- Vertebral body
- Pedicle
- Lamina
- Spinous process
- Spinal central canal
- Lateral recess
- Neuroforamen (intervertebral foramen)
- Facet joint:
- Inferior articular process (medial)
- Superior articular process (lateral)
- Ligamentum flavum (connects laminae)
- Vertebral artery
- Carotid artery
- Jugular vein
- Kidney in thoracic MRI
- At C1 Odontoid level: alar ligaments, transverse ligament
Spinal injury trauma and instability:
Spinal stability:
The ability to protect from neurological injury when the spine is exposed to physiological loads under normal range of motion.
Unstable spine:
- 2 contiguous columns affected by Denis classification (see below)
- High score on Thoracolumbar Injury Classification and Severity Score (TLICS, see below)
- Translation of >2mm (indicates injury to ligaments)
- Widening of facet joints
- Widening of interspinous spaces
- Disruption of posterior vertebral body line
- Loss of >50% of vertebral body height
- >20% of kyphosis
Denis classification:
- Three column concept of spinal stability: Unstable spinal injury is present when 2 contiguous columns are affected.
- Anterior column:
- Anterior longitudinal ligament (ALL)
- Anterior 2 thirds of the vertebral body and intervertebral disc.
- Middle column:
- Posterior 1 third of the vertebral body and intervertebral disc
- Posterior longitudinal ligament (PLL).
- Posterior column:
- Everything posterior to PLL
- Includes: pedicles, facet joints, articular processes, ligamentum flavum, neural arch (posterior arch) and interspinous ligaments.
Thoracolumbar Injury Classification and Severity Score (TLICS):
Higher points mean worse injury and suggests intervention.
Based on 3 components:
- Injury morphology
- Integrity of the posterior ligamentous complex (PLC)
- Neurologic status of the patient
Thoracolumbar Injury Classification and Severity Score (TLICS)
- Injury morphology:
- Compression 1 point
- Burst 2 points
- Translation or rotation 3 points
- Distraction 4 points
- Integrity of the posterior ligamentous complex (PLC):
- Intact 0, points
- Injury suspected or indeterminate 2, points
- Injured 3, points
- Neurologic status of the patient:
- Intact 0, points
- Nerve root involvement 2, points
- Spinal cord or conus medullaris injury:
- Incomplete 3, points
- Complete 2, points
- Cauda equina syndrome 3, points
- TLICS Score Treatment Recommendation:
- 0–3 Nonsurgical
- 4 Nonsurgical or surgical
- ≥5 Surgical
Posterior ligamentous complex (PLC):
- Ligamentum flavum
- Articular facet capsules
- Interspinous ligaments
- Supraspinous ligament (connects the tips of the spinous processes from C7 to the sacrum)
MRI features of Posterior ligamentous complex (PLC) injury:
- Loss of integrety of the ligamentum flavum or supraspinous ligament (discontinuation of hypointense stripe sagittal T1, sagittal T2).
- Interspinous ligament change (hyperintensity on sagittal T2, sagittal STIR).
- Facet edema or fluid (hyperintensity on axial T2, axial STIR).
CT features of Posterior ligamentous complex (PLC) injury (MRI can visualize the PLC directly):
- Interspinous distance widening (splaying of the spinous processes)
- Facet joint widening
- “Naked” empty facet joints, “perched” dislocated facet joints,
- Spinous process fracture (avulsion fractures of the tips of the spinous processes due to supraspinous ligament injury)
- Vertebral subluxation or dislocation
Degenerative changes, disc disease and spondylosis:
- Superiorly: pedicle for vertebra above.
- Inferiorly: pedicle for vertebra below.
- Anteriorly (ventrally): intervertebral disc and vertebral body.
- Posteriorly (dorsally): facet joint.
- Laterally: Extraforaminal space.
- Medially: the lateral recess of the spinal canal.
- Superiorly: continues as the lateral recess.
- Inferiorly: continues as the lateral recess.
- Anteriorly (ventrally): intervertebral disc and vertebral body
- Posteriorly (dorsally): articular facet.
- Laterally: neuroforamen, pedicles of the vertebrae,
- Medially: the central portion of the spinal canal, spinal cord.
- Superiorly: continues as the spinal canal.
- Inferiorly: continues as the spinal canal.
- Anteriorly (ventrally): intervertebral disc and vertebral body
- Posteriorly (dorsally): ligamentum flavum, lamina of the vertebra (vertebral arch).
- Laterally: the lateral recess.
- Compression of central spinal canal: graded no stenosis, mild stenosis <1 third, moderate stenosis 1 to 2 thirds, severe stenosis >2 thirds.
- Reduction of anterior CSF space
- Reduced or absent fluid around cauda equina
- Hypertrophy of ligamentum flavum
- Epidural lipomatosis
- Reduction of posterior epidural fat
- Nerve root sedimentation sign
- Redundant nerve roots of cauda equina
- Compression of subarticular zone: graded no stenosis, mild stenosis <1 third, moderate stenosis 1 to 2 thirds, severe stenosis >2 thirds.
- Visible nerve root compression in lateral recess
MRI features of neuro-foraminal stenosis:
- Perineural intraforaminal fat reduction
- Compression of foraminal zone
- Hypertrophic facet joint (degenerative)
- Foraminal nerve root impingement/compression
- Size and shape of foramen is reduced
Retrolisthesis:
By definition retrolisthesis is a movement (subluxation) of >=2mm of the vetebral body posteriorly in relation to the vertebral body below it.
Retrolisthesis grading:
- Can be graded my measuring the retrolisthesis in mm.
- Can be graded by the intervertebral foramina IVF method:
- Divide the intervertebral foramina into into 4 equal units.
- Grade 1 posterior displacement of up to 25% of the IVF
- Grade 2 posterior displacement of 25% to 50%
- Grade 3 posterior displacement of 50% to 75%
- Grade 4 posterior displacement of 75% to 100
Retrolisthesis classification:
- Complete Retrolisthesis: The body of the subluxed vertebra is is posterior to both the body of the vertebra above as well as the segment below
- Stair stepped Retrolisthesis: The body of the subluxed vertebra is posterior to the body of the vertebra above but is anterior to the one below.
- Partial Retrolisthesis: The body of the subluxed vertebra is posterior to the body of the vertebra segment either above or below.
Assess vertebral endplates degenrative changes (Modic changes):
- Modic Type 1:
- T1 Dark
- T2 Bright
- Marrow edema, inflammation
- Modic Type 2:
- T1 Bright
- T2 iso or bright
- Hematopoietic (Red) marrow to fatty (yellow) marrow conversion
- Modic Type 3:
- T1 Dark
- T2 Dark
- Subchondral bony sclerosis
Consider malignant lesions when:
- Posterior elements are involved
- Signal change involves the entire vertebral body
- Lytic lesions are present
- Surrounding soft tissues changes are present
- Multiple lesions are present
Sequences and signal characteristics:
Also see MRI brain notes
T1:
- CSF & Disc spaces are hypointense
- Vetebral bodies contain fat (hyperintense), metastasis replace this and become hypointense
T2, fast spin echo FSE:
- Excellent for delineating CSF space, nerve roots and spinal cord edge
STIR:
- Excellent for ligamentous injury
- Excellent for multiple sclerosis spinal cord lesions
- Excellent for gliosis or edema in the spinal cord
- Excellent for acute vertebral body fracture (bone edema)
GRE:
- Exaggerates stenosis & bony lesions
- On 3T can give good visualization of multiple sclerosis lesions
References:
- Mamisch N, Brumann M, Hodler J, Held U, Brunner F, Steurer J; Lumbar Spinal Stenosis Outcome Study Working Group Zurich. Radiologic criteria for the diagnosis of spinal stenosis: results of a Delphi survey. Radiology 2012; 264:174–179
- Gustav Andreisek G, Imhof M, Wertli M, Winklhofer S, Pfirrmann C, Hodler J, Steurer J; Lumbar Spinal Stenosis Outcome
- Study Working Group Zurich. A Systematic Review of Semiquantitative and Qualitative Radiologic Criteria for the Diagnosis of Lumbar Spinal Stenosis. AJR 2013; 201:W735–W746