Similar to CT a systematic approach is best when interpreting MRI brain. MRIs of the brain can be intimidating at first sight because of all the different sequences and parameters. However, the same general principles of CT head interpretation apply, as the first steps are anatomically-based after all. After that you can add an understanding of what each MRI sequence is designed for and how it changes the appearance of normal structures and abnormal findings. Lastly, you can delve in the world of MR physics to gain an enlightened view of MR. But that last step is far beyond the scope, or ability, of this website!!
As with CT, you’ll have to hit the books, review articles and original research and interpret thousands of studies to get the real expertise, but here’s a start! Get into the good habit of trying to interpret your own patients imaging and then comparing it with the expert report.
Description:
Describe the following:
- Patients name, date of birth
- Comparison study
- Technical features: what sequences were acquired, with or without contrast
- The general normal structures (systematically)
- The abnormal findings
- Then interpret the findings to arrive at a differential diagnosis. Summarise the take away points under Impression.
Approach to the structures, sagittal:
Scroll and look at midline image (in the mid-sagittal plane) from bottom to top. Then look laterally at the parasagittal planes. Observe the normal and abnormal structures.
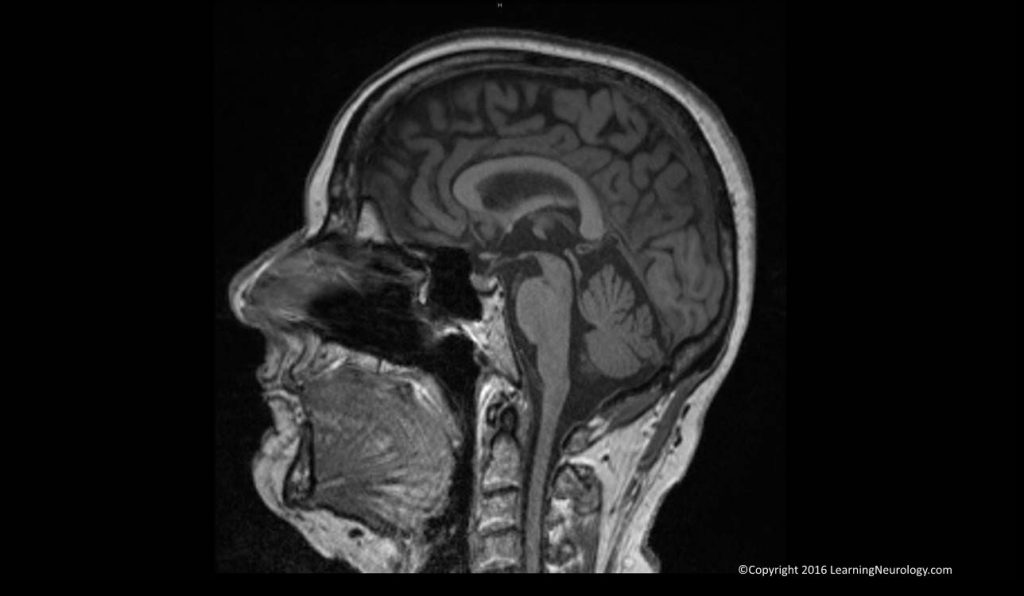
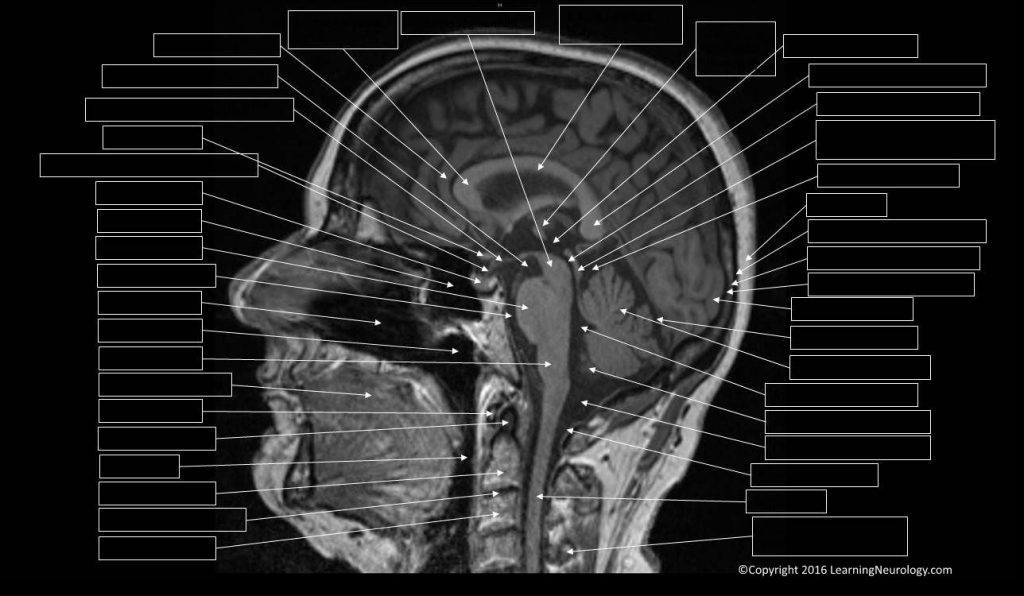
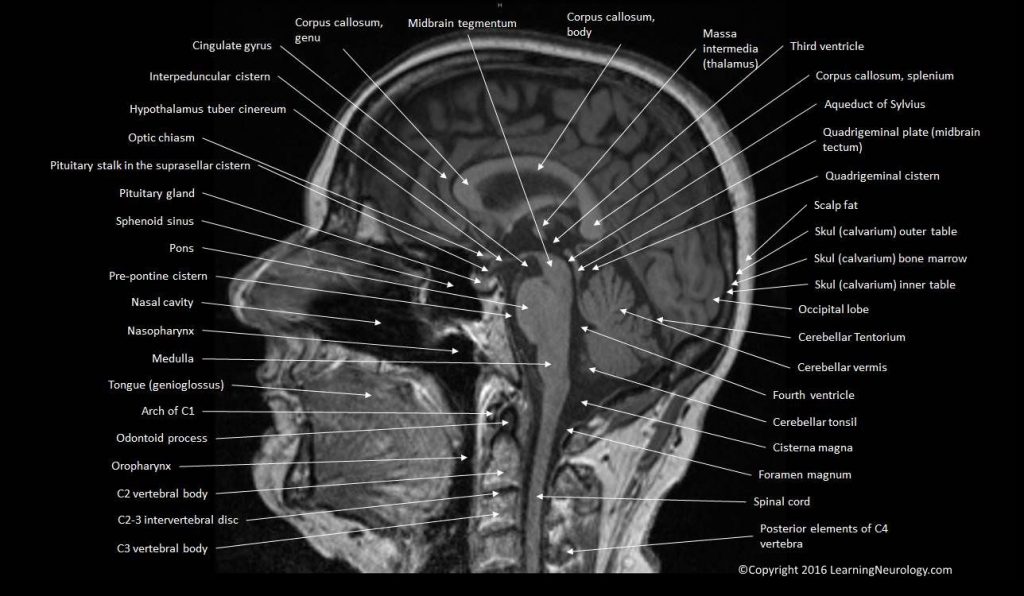
Look at midline image, from bottom to top:
First, look at the mid-sagittal plane:
- Cervical spinal cord and cervical spine
- Foramen magnum & base of skull
- Cerebellar tonsils
- Fourth ventricle
- Cerebellar vermis
- Brain stem
- Basilar artery
- Sella, pituitary & optic chiasm
- Corpus callosum
- Cingulate gyrus
- Cortex
- Superior sagittal sinus
- Review areas:
- Orbits
- Sinuses: Ethmoid, sphenoid, and frontal
- Nasopharynx, Oropharynx
Then, look laterally at parasagittal planes:
- Hemispheres
- Extraxial collections
- Carotid & vertebral arteries
- Review areas:
- Transverse sinuses
- Sinuses: frontal, ethmoid, sphenoid, mastoid, maxillary
- Internal auditory canals IAC
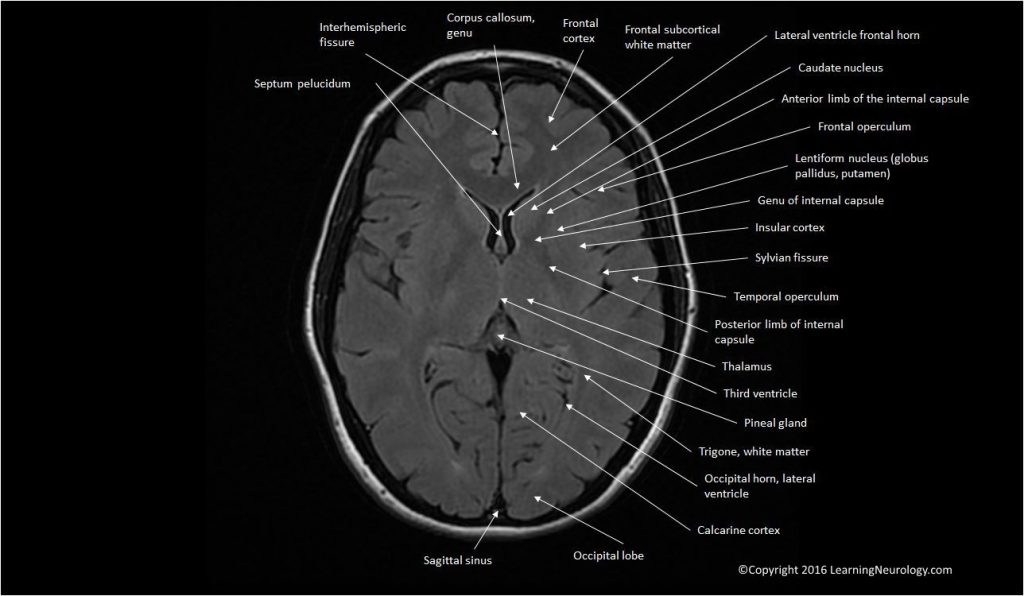
Approach to the structures, axial:
When interpreting the axial images follow a systematic approach. Scroll through the MRI from bottom to top interpreting each of these systems or areas at a time. The CSF system (ventricles, cisterns and sulci), the brain matter (grey matter structures and white matter structures), the vessels and venous sinuses, the meninges and skull and adjacent tissues. And finally the extended search i.e. review areas (paranasal sinuses, pituitary, orbits, nasal cavity nasoparhynx and oropharynx).
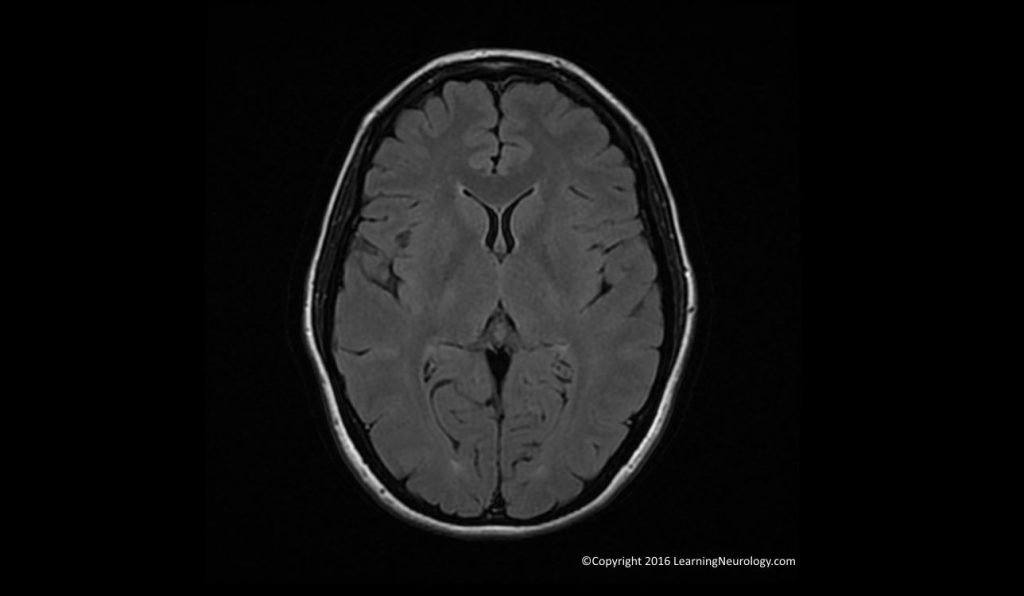
Ventricles, cisterns & sulci:
- When ventricles, cisterns, fissures or sulci are ‘squashed” we used the term effaced. When they are large we just describe them as large or enlarged. Theses different CSF spaces should be interpreted together for example, effaced sulci tell us that the enlarged ventricles likely represent hydrocephalus. Whereas enlarged sulci would inform us taht the enlarged ventricles likely represent brain volume loss i.e. atrophy.
- Ventricles:
- Lateral ventricles (frontal, occipital & temporal horns), Third ventricle (slit like), fourth ventricle
- Cisterns & fissures:
- Quardrigeminal plate cistern, interpeducular cistern, ambient cistern a.k.a. cistern of the great cerebral vein
- Sulci:
- Appearance: effaced, obscured
- Ventriulo-sulcal proportionality
Brain matter, Grey & white matter:
- Midline shift
- Grey white differentiation
- Structures:
- Caudate nucleus, Internal capsule, Putamen & globus pallidus, thalamus.
- Other structures: centrum semiovale, midbrain, pons, medulla, cerebellum
Vessels arteries, veins & venous sinuses:
- Arteries: basilar, carotid arteries, vertebral artery, middle cerebral arteries
- Superior sagittal sinus, torcula, transverse sinus, sigmoid sinus, internal jugular vein
Meninges:
- Dural involvement/enhancement look at (falx, tentorium, CP angle)
- Leptomeningeal enhancement look at (basal cisterns, cerebellar folia, sulcal perivascular spaces)
Extended search:
- Sella, pituitary & optic chiasm
- Paranasal sinuses (ethmoidal, sphenoid, frontal, mastoid), temporal bone/ears
- Orbits
- Nasopharynx, Oropharynx
Editor note:
Interpretation:
Basic notes on Sequences and Signal characteristics:
T1 and T2:
- On T1: white matter appears white & grey matter appears grey & CSF is black
- T2 is the opposite.
- On T2: the thalamus is darker than the corpus striatum (putamen & caudate) which are darker than cortical grey matter.
T1 hyperintense (bright) lesions i.e. short T1 lesions:
- High protein: e.g. Rathke cleft cyst
- Calcium
- Fat & cholesterol
- Subacute hemorrhage:
- Subacute thrombus
- Manganese (e.g. in striatum in liver disease)
T1 hypointense (dark) lesions i.e. lesions with T1 prolongation:
- CSF
- Edema
- Chronic hemorrhage
- Air
- Fast flow in blood vessels
- Low protein
T2 hyperintense (bright) lesions i.e. long T2:
- T2: sensitive for many pathologies, edema or gliosis
- Edema
- Gliosis
- CSF
T2 hypointense (dark) lesions i.e. short T2:
- Calcification
- Air
- Fibrous tissue
- Acute hemorrhage
- Very chronic hemorrhage
- High protein
- Calcium
- Fast flow in blood vessels
- Metal
FLAIR (fluid-attenuated inversion recovery):
- a type of T2 but CSF is black.
- FLAIR: shows areas next to CSF (periventricular) very well. Also good for juxtacortical areas. Inferior quality to other sequences in posterior fossa and spinal cord.
T1 +Gadolinium +DTPA:
- shows BBB disruption
Functional MRI (fMRI):
- uses Blood Oxygenation Level Dependent BOLD contrast
PD proton density:
- grey matter has high signal, white matter has low signal, CSF is black
DWI diffusion weighted imaging:
- uses diffusion of water molecules. Calculates apparent diffusion coefficient ADC that can be displayed on a separate scan.
- detects changes in local deoxy- and oxy-hemoglobin ratios, helps localise cognitive (including language) & other functions
- high signal in acute ischemic stroke, encephalitis, focal seizure
Apparent diffusion coefficient, ADC:
- Decreased in cytotoxic oedema i.e. opposite to diffusion i.e. true DW restriction i.e. infarct or abscess.
- Increased from a T2 effect ‘T2 shine-through’ i.e. same as diffusion.
- Restricted diffusion= high signal on DWI & low signal on ADC
Time of flight MRA (TOF MRA):
- Doesn’t require contrast
Gradient echo GRE MRI:
- Detects hemorrhage (hemosiderin) well in delayed presentation of stroke. Low intensity (called susceptibility artifact or T2* effect).
Dynamic MRA:
- Requires contrast but is good quality
STIR short tau inversion recover MRI:
- a T2 MRI that suppresses fat & retains T2 weighting
Miscellaneous interpretation notes:
Myelination:
- Mature myelin pattern by 18 months.
- Subcortical U fibers myelinate around 8 months of life.
- At birth Major sensory & motor systems have myelin.
Other pointers:
- To notice hyperintensities in the caudate & putamen, compare them to the cortex, they shouldn’t be hyperintense.
Normal variants:
- Virchow Robin spaces in the basal ganglia may be confused for lacunar infarcts: they contain CSF and are isointense to CSF i.e. hypointense on T1 & PD & FLAIR, hyperintense on T2.
- Occipital horns may be asymmetric
Normal structures that enhance:
- Venous sinuses
- Adenohypophysis and pituitary stalk
- Choroid plexus
- Area postrema
Causes of T1 hyperintensity:
- High protein: E.g. Rathke cleft cyst
- Calcium
- Fat & cholesterol
- Subacute hemorrhage:
- Subacute thrombus
- Manganese (e.g. in striatum in liver disease)
Causes of T1 hypointensity:
- CSF
- Oedema
- Chronic hemorrhage
- Air
- Fast flow in blood vessels
- Low protein
Causes of T2 hyperintensity:
- CSF
- Oedema
Causes of T2 hypointensity:
- High protein
- Acute hemorrhage
- Chronic hemorrhage
- Calcium
- Fast flow in blood vessels
- Metal
Causes of localised cerebral oedema:
Cytotoxic (abnormal restricted diffusion):
- Infarction (stroke)
- Abscess, empyema, infection
- Uncommonly demyelination
Vasogenic (unrestricted diffusion):
- Tumours
- Reversible posterior leukoencephalopathy
Interstitial:
- Hydrocephalus (transependymal edema)
Seizure related changes:
- Cortical involvement,
- Spares the white matter
- Can revert after seizure control
- Not confined to vascular territory
- May involve “basal ganglia”
- May involve the thalamus
Causes of bilateral thalamic lesions:
- Vascular:
- Venous thrombosis
- Thalamic infarcts (artery of Percheron)
- Venous congestion
- Neoplastic:
- Lymphoma
- Astrocytoma
- Encephalitis
- nvCJD
- Wilson’s disease
- Hemochromatosis
- Hemolytic uremic syndrome
- Osmotic demyelination
- Methanol poisoning
- Enzyme deficiencies:
- Tay-Sach disease
- Sandhoff’s disease (beta-hexosaminidase deficiency)
Causes of hyperintense CSF in sulci or cisterns on FLAIR:
- SAH
- High protein (meningitis, neoplastic)
- High oxygen tension (intubation & ventilation)
Diffuse white-matter injury:
- Symmetrically infiltrative tumors
- Hereditary white-matter diseases
- Metabolic injury:
- Anoxia, carbon monoxide poisoning, mitochondrial disorders
- Exposure to a white-matter toxin:
- Vaporised heroin
- Cocaine
- Solvants
- Asymmetric or multifocal injury:
- Vascularly mediated
- Inflammatory disorders
- Infections
- Radiation injury